Why see a psychologist ?
There are many reasons you might consider seeing a psychologist, from wanting help setting goals or making changes in your life, to getting assistance dealing with more complex or persistent problems affecting your everyday life. Regardless of the issues you are facing, it can be hard to ask for help or even sometimes recognize or admit that help is needed. However, there is no shame in admitting that you need help and the sooner you begin working toward change, the sooner you can begin moving on with your life.
Some common reasons for seeing a psychologist include: difficulties with school or job demands, learning/developmental disabilities, neurological impairments (e.g., Parkinson’s disease, multiple sclerosis), stroke / transient ischemic attack (TIA), brain injury, concussion, chronic health / medical conditions (e.g., diabetic neuropathy, epilepsy), issues related to aging (i.e., normal aging, mild cognitive impairment, dementia), low self-esteem, anxiety, excessive worry, stress, discomfort in social situations, phobias/fears, obsessive and/or compulsive behaviours, difficulty sleeping, body image issues, and eating disorders.
If you are unsure whether your particular concern or issue warrants psychological intervention, there is no harm in calling to find out. A meeting can be booked in which we can discuss the issue(s) in more depth and together we can arrive at the best course of action.
What is a psychologist and how does it differ from a psychiatrist or a counsellor/therapist?
The primary differences between psychologists and psychiatrists relates to their level of education and the focus of their training. A psychologist has completed an MA or a PhD in psychology, which entails 6-10 years of specialized training and education in the nature of human thoughts, feelings and behaviour. As part of this training, psychologists also receive advanced training in the provision of various types of psychotherapy. Those who have completed a PhD may call themselves “Dr.”; those who terminated their training after obtaining an MA are called Psychological Associates. In order to use the title of Psychologist or Psychological Associate, a practitioner must be registered with the College of Psychologists of Ontario. In addition, all psychologists must declare their areas of specialized training which detail the type of psychology they practice as well as the age groups they serve. Upon registering with the College of Psychologists of Ontario (CPO), or other provincial regulatory bodies, they must practice only within their areas of declared competency. Psychologists are the only professionals qualified in the use of certain kinds of tests and assessment measures. Although psychologists often have a working knowledge of medications, they are not currently licensed to prescribe medicine in the Province of Ontario.
A Psychiatrist, by comparison, is a medical doctor who specializes in mental health. Typically, their focus is on the biological aspects of mental health, as opposed to the psychotherapeutic aspects, and thus they often use medication to treat different mental health problems. While some psychiatrists do have training and experience in the provision of psychotherapy, the nature and degree of this training is often quite different from that of psychologists. Psychiatrists are registered with the College of Physicians and Surgeons of Ontario.
The term “therapist” does not indicate the type or degree of education and training attained by a person providing services. Practitioners who go by the title of “counsellor”, “therapist”, “life coach”, or other similar titles are examples of unregulated service providers. For more information on regulated versus unregulated service providers, please see the section entitled “Why see a regulated psychologist / health professional?”
What is a neuropsychologist?
A neuropsychologist is a clinical psychologist whose area of expertise deals with the relationship between the brain and behaviour. A neuropsychologist’s practice involves assessment, diagnosis, treatment planning and, in some cases, therapy and/or rehabilitation of individuals who have sustained any type of injury (or suspected injury) to the brain. In order to declare competency as a neuropsychologist, practitioners much have earned a PhD in psychology from an accredited university program, completed a minimum two years of training and supervision in a neuropsychological practice, completed an accredited internship placement (or the equivalent), and passed all mandatory examinations to become licensed for independent practice in their state or province.
Why see a regulated psychologist / health professional?
In Ontario, psychologists are regulated health professionals registered with the College of Psychologists of Ontario (CPO) to practice psychology and governed by the Regulated Health Professionals Act and the Psychology Act, 1991. Only practitioners registered with the CPO can call themselves “psychologists”. Becoming a registered psychologist is a highly structured process in which a candidate must meet several requirements, including completing a PhD in Psychology, completing a one-year post-doctoral internship and one year of supervised practice, during which time several written and oral examinations on jurisprudence, ethics and the profession of psychology must be completed. Successful candidates must follow the Canadian Code of Ethics for Psychologists, as well as the Standards of Professional Conduct as stated in the Regulated Health Professional Act for the Province of Ontario. Psychologists are trained more generally in the assessment, diagnosis and treatment of mental health issues, although many have areas of concentrated experience and training. Members of the CPO must state their areas of declared competence, and only practice within those areas declared. All members of the CPO are required to attend workshops, conferences and seminars in order to ensure continual professional development.
By seeing a registered psychologist, a regulatory body monitors the professional and ethical standard of conduct of its members and is responsible for protecting the interests of the public by holding members accountable for their actions and the services they provide. By comparison, there is no minimum level of education or training for unregulated service providers, no way to formally verify credentials of service providers, and there is no regulatory body with legal authority to protect the interests of the public should any disputes arise. Practitioners who go by the title of “counsellor”, “therapist”, “life coach”, or other similar titles are examples of unregulated service providers.
You can verify that a practitioner is regulated and that he or she is in good standing by calling the CPO or by visiting the website (www.cpo.on.ca), which lists every member of the College, their standing, their areas of declared competence, and their current practice.
What should I expect at my first therapy appointment?
The first appointment for therapy is largely geared towards information gathering and getting to know each other a little bit. We will discuss what Cognitive Behavioural Therapy (CBT) is, how it works, and how therapy sessions will be structured, and we will talk briefly about the issue(s) that have brought you in to see me. We will also discuss limits of confidentiality and privacy, and any questions or concerns you may have will be answered. A consent form will be completed indicating in writing that you have given informed consent to enter into treatment after which an interview will be conducted to gather some background information that will be used to help determine any diagnoses (if appropriate) and to guide treatment.
As CBT is an active and collaborative process, we will sit together to discuss issues and work on material together. Therapy sessions last 50 minutes and sessions are scheduled approximately one week apart.
What should I expect when I come in for an assessment?
At the start of your assessment appointment, we will take some time to briefly discuss the nature of the issue(s) you have been experiencing and the type of the assessment you will undergo. Once that has been established, we will begin the process of informed consent in which I will explain to you issues and limits of confidentiality and privacy, what type of information will be gathered, how that information will be used, and your rights to access that information. I will explain briefly the nature of testing (i.e., what you will be asked to do, how long it will take, and when the results will be ready). You will also have the opportunity to ask any questions and we can discuss any concerns you may have. If all your questions and concerns have been addressed to your satisfaction and you agree to proceed with the assessment, we will both sign an informed consent form (and we will both keep a copy) and the assessment will begin with a clinical interview lasting approximately 1-2 hours. The information gathered is used to help determine appropriate tests to administer, to assist with interpretation of test results and to guide treatment recommendations. All tests are standardized measures designed to accurately assess cognitive functioning. Testing will include completing paper-and-pencil type measures, filling in questionnaires, putting things together, listening to or looking at materials and answering questions.
Depending on the type of assessment, testing will last from 3-8 hours; you will be informed of the expected duration of the assessment at the outset. Upon completion of the assessment, the tests will be scored and interpreted, and results should be available within one month’s time. A report will be drawn up which includes a summary of your relevant background information, the results of tests, any diagnoses (if relevant), and treatment recommendations. Once this report has been completed, we will meet again to go over the results and discuss the treatment plan. If you were referred for an assessment by a third party, a copy of the report will be sent to the referring source. A copy of the report will also be kept in your file.
What is Cognitive Behavioural Therapy (CBT)? How does it differ from traditional psychotherapy?
Cognitive Behavioural Therapy (CBT) is an evidence-based form of therapy that differs from traditional psychotherapy in that it is a structured, short-term, goal-directed, problem-focused, and active form of therapy. CBT is based on the realization that our thoughts (the “cognitive” part of CBT) can influence our feelings and behaviour about a given situation or event, and vice versa. Such thoughts are typically negative (e.g., “I can’t succeed in my new job”; “nobody will ever want to be my friend”; “I should have known better) and they happen so quickly that we are usually not even aware that such thoughts crossed our minds; we call these “automatic thoughts”, and they represent a distorted way of thinking about and perceiving experiences or events. CBT is a collaborative approach in which the client and therapist work together in a supportive and respectful manner, with the therapist helping the client to learn to recognize his or her patterns of behaviour and distorted thoughts, and to learn and practice new ways of thinking about, feeling about, and acting towards different situations and events in a safe environment. A major advantage of CBT is that the client learns how to be his or her own therapist, which is a useful tool in preventing relapse.
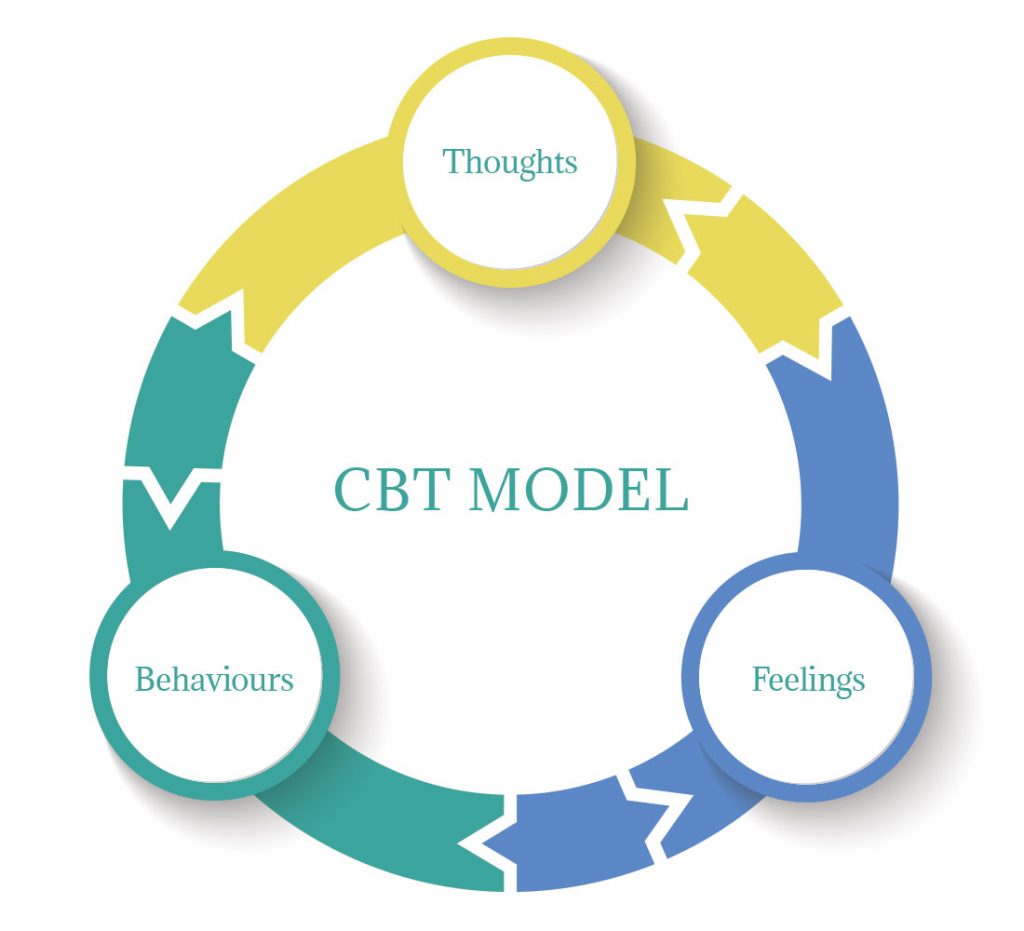
CBT model demonstrating the reciprocal influence that thoughts, feelings and behaviours can have on each other.
An additional advantage of CBT as a treatment choice is that it does not require the use of medication in order to be effective. In fact, research has consistently shown that CBT is not only an extremely effective method for treating many types of psychological problems, such phobias, anxiety, panic attacks/panic disorder, obsessive-compulsive disorder (OCD), social anxiety, post-traumatic stress disorder (PTSD), anger issues, sleep and eating disorders, and chronic pain and illness, amongst others, but also that in some cases it is more effective than medication. It should be noted, however, that medication may, in certain cases, help an individual be able to more easily manage their anxiety levels and mental health problems in order to allow them to engage in the therapeutic process. If, through working together, it seems that medication may be helpful to ensure the best treatment, we can discuss various options and with your written permission I can work with your family physician to help establish the best care. Although psychologists typically have a working knowledge of various psychotherapeutic medications, at the present time we are not licensed to prescribe medication in the province of Ontario.
How long does therapy take? How many sessions will I need?
A standard course of CBT lasts 12 sessions, but there are times when fewer or more sessions are required. Remember that CBT is a collaborative process and therefore much depends not only on how each session goes but also on how treatment progresses in between sessions through the completion of homework. Ultimately, it is the client who must make changes in his or her life; my job is to help you get there.
How much does it cost to see a psychologist, and who pays for psychological treatment?
Unfortunately, fees for psychological assessment and/or treatment are not covered by OHIP. However, many people have extended health plans that provide full or partial coverage for services provided by registered psychologists. At the end of each therapy session or upon the completion of an assessment, the client will receive an itemized receipt detailing the costs associated with each service. These receipts may be submitted by the client to his or her insurance company for reimbursement, if applicable. Treatment and assessment services are charged by the hour, with an hourly rate set in accordance with the guidelines set out by the Ontario Psychological Association (OPA). Accepted methods of payment include cash or cheque.
Is there a cancellation or missed appointment fee?
There are no fees for cancelled appointments provided that a minimum of 24 hours notice is provided. Missed therapy appointments or therapy appointments cancelled with less than 24 hours notice are subject to a $75 fee; missed assessment appointments or assessment appointments cancelled with less than 24 hours notice are subject to a $100 fee. There are no fees associated with rescheduling therapy sessions or assessment date provided 24 hours notice is given.
Do you do phone or Skype therapy sessions?
In certain instances, telepsychology (i.e., phone sessions) are available, as are video sessions. Please inquire for further information if interested in such forms of treatment are preferred.
Are your services confidential?
Yes. Any personal information that is collected is kept secure and remains confidential. Personal information includes any information about you as a person, including characteristics (e.g., age, gender, income, education, address/contact information), health information, capacity to make decisions, and personal beliefs or views. Any such information that is collected is used and disclosed only to the extent necessary for services to be provided. At no point in time during treatment/assessment will your personal information (including topics discussed or even whether you are in treatment) be released to anyone, including other treating physicians/clinicians, insurance companies, legal representatives or family members without your written consent. There are, however, a few exception to the limits of confidentiality in which information would be shared without your prior written consent. Such instances do not arise frequently but they would necessitate releasing information in order to keep you or the public safe. Instances in which confidentiality could be broken are as follows:
1. If there are concerns about a child being harmed, abused or neglected, or if there are concerns about a child being at risk for harm, abuse or neglect
2. If you report having thoughts or intent for suicide or causing serious harm to another person(s)
3. If you report having been sexually abused by another health care practitioner (e.g., a doctor, dentist, nurse, etc).
4. If there is a court order or subpeona from a judge for release of information
Psychologists are required to keep records for 10 years, after which they are destroyed.
Do I need a referral from my doctor?
A doctor’s referral is not required to seek treatment – you may self-refer simply by calling to book an appointment. If your health benefit provider / insurance company requires a physician’s referral before they will reimburse you, your doctor can submit the required paperwork.
What age groups are you licensed to treat?
My areas of declared competency are neuropsychology and clinical psychology, and I am licensed to work with adults 18 years of age or older. I also have a specialized declared competency to work with senior citizens for both assessment and treatment.
I am not licensed to treat or assess children or adolescents but would be happy to make an appropriate referral on your behalf if you are seeking treatment for individuals under the age of 18.
Dr. Kristen Kaploun Office
Dr. Kristen Kaploun Office
1100 Burloak Drive, Ste. 300
Burlington, ON L7L 6B2
Get Directions
Tel: 289-983-7570
Fax: 905-332-3007
Building is wheelchair accessible
Plenty of free parking onsite
If this is an emergency, please visit your local hospital’s emergency department, or call 911.
Joseph Brant Memorial Hospital
1230 North Shore Blvd.
Burlington, ON L7S 1W7
905-632-3737
If you cannot find the answers to any questions you may have, or if you're not sure whether we can help, please do not hesitate to contact us by phone or email. We will make every effort to return all calls or emails within 48 hours of initial contact, and from there we can set up an initial appointment.
Other local crisis hotlines and resources are listed below:
Burlington Telecare Distress Line
905-681-1488
(24 hours)
Crisis Outreach and Support Team (COAST)
1-877-825-9011
note: this is not an emergency service
North Halton Distress Centre:
905-877-1211
Oakville Distress Centre:
905-849-4541
Emergency Psychiatric Services at St. Joseph’s Healthcare, Hamilton:
905-972-8118
Hamilton 24 Hour Crisis Line:
905-972-8338
